Goal Area 3: Promoting Quitting
 The SUTPP and the CDC share the goal of reducing the health burdens of commercial tobacco and nicotine use by promoting and supporting quitting among adults and young people.
The SUTPP and the CDC share the goal of reducing the health burdens of commercial tobacco and nicotine use by promoting and supporting quitting among adults and young people.
In this section, we explore smokers’ desire to quit and quit attempts. We look at awareness of quitlines (for all tobacco and nicotine users, including current ENDS users), use of quit aids, and barriers to quitting. This section also covers commercial tobacco and nicotine users’ visits to healthcare providers and conclusions and recommendations based on the data and best practices in helping people quit.

Efforts to Quit Smoking
Smokers’ Desire to Quit
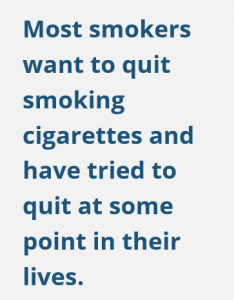
More than half of smokers (57%) wanted to quit smoking cigarettes (Figure 16). The 11-point difference between 2019 and 2021 for smokers who want to quit was not significant, probably because relatively few people answered the questions. There were no significant changes from 2015–2021.
Smokers’ Quit Attempts
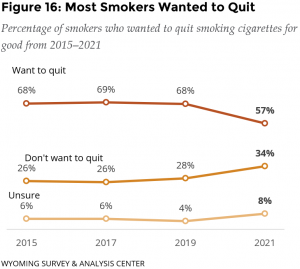
 At some point in their lives, about four out of five current smokers (82%) had stopped smoking for at least one day because they were trying to quit for good.
At some point in their lives, about four out of five current smokers (82%) had stopped smoking for at least one day because they were trying to quit for good.
About one third (32%) of current smokers have tried to quit smoking at least once in the past year because they were trying to quit for good (Figure 17).
Smokers’ quit attempts have not changed significantly between 2010 and 2021.
Aids to Quit Smoking
Awareness of Quitlines

Most commercial tobacco and nicotine users (including ENDS users, 68%) were aware of telephone quitline services (Figure 18). About half (49%) of non-tobacco and non-nicotine users were aware of telephone quitline services.
This may demonstrate the success of media campaigns by SUTPP and their partners, including county-level efforts.
Smokers’ Use of Quit Aids

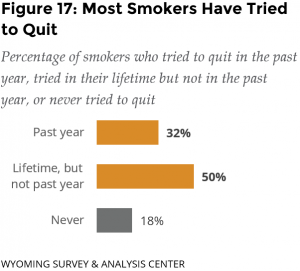
Most (54%) smokers who tried to quit in the last year used at least one quit aid. Nicotine re-placement therapy (NRT) was the most popular aid used by smokers (Figure 19). This may have included people buying them over the counter or getting them from the Wyoming Quit Tobacco (WQT) program.
Smokers’ Obstacles to Quitting Cigarettes
Cravings for a cigarette was the most common obstacle for current smokers the last time they tried to quit (75%; Figure 20). Current smokers said other obstacles to quitting cigarettes included the loss of a way to handle stress (65%) and worsening anxiety (50%). For smokers, the loss of a way to handle stress has decreased significantly over time from 2017 to 2021. Other barriers have been relatively stable over the same timeframe.
The WQT program specifically targets the most common barriers to quitting smoking (https://www.quitwyo.org). In particular, the medications provided are designed to reduce cravings. Coaching can include strategies to deal with other barriers.

Health Professionals’ Involvement in Quitting Commercial Tobacco and Nicotine Use
Visits with Health Professionals
The 2021 ATS asked respondents if they had seen a health professional (a doctor, dentist, nurse, or other health professional) in the past year and if so, if the health professional asked if they smoked cigarettes or used any other tobacco product or nicotine products, including ENDS.
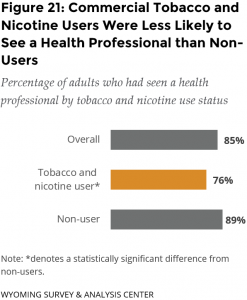
Most commercial tobacco and nicotine users had seen a health professional in the past year (76%; Figure 21). Still, commercial tobacco and nicotine use was related to lower likelihood of seeing a health professional. This difference might be due, in part, to barriers to seeking care that might be linked to tobacco and nicotine use, such as lower income.
Health Professionals’ Support for Quitting Tobacco and Nicotine Use
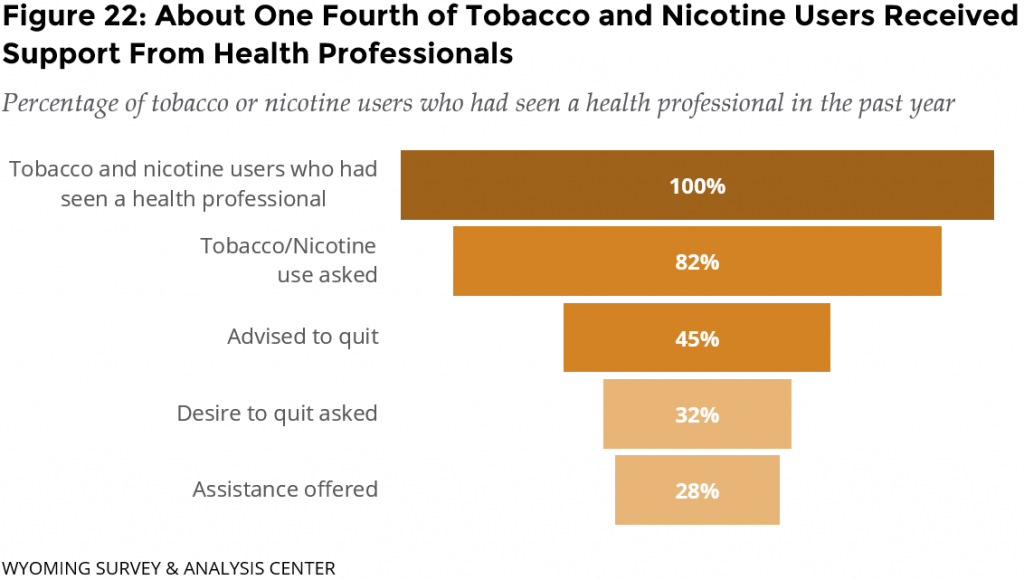
Adults are often asked about their commercial tobacco or nicotine use when visiting a health professional:
- 72% of all adults were asked if they smoked cigarettes or used any other tobacco or nicotine products.
- 82% of tobacco or nicotine users were asked if they smoked cigarettes or used any other tobacco or nicotine products, significantly more than 67% for non-users.
We do not know to what extent health professionals use medical records to identify tobacco and nicotine users (and non-users) during a visit. This may be a limitation when health professionals had records of their patients’ tobacco or nicotine use and did not ask if they used tobacco or nicotine products.
Less than half of tobacco and nicotine users received support with quitting, even when focusing on those who say a professional asked them about their tobacco or nicotine use (Figure 22).
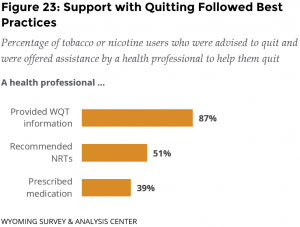
When commercial tobacco or nicotine users were offered assistance, health professionals pro-vided WQT information (87%; Figure 23), recommended NRTs (51%), and prescribed medication (39%). These protocols align with best practices in support of quitting.
Conclusions
Most smokers want to quit smoking cigarettes and have tried to quit at some point in their lives. When they try to quit or want to quit, smokers face obstacles such as cravings for a cigarette, loss of a way to handle stress, and worsening anxiety. The WQT program is designed to assist with these obstacles. Media emphasizing how the WQT program addresses common barriers to quitting smoking may increase enrollment in the WQT program.
Most tobacco and nicotine users are aware of quitline services. Most who had tried to quit in the last year used a quit aid the last time they tried to quit.
Visits to health professionals are opportunities for connecting current commercial tobacco and nicotine users to available resources and to address barriers to quitting. Most adults were asked by a health professional if they used commercial tobacco or nicotine products. Adult commercial tobacco and nicotine users were less likely to report that health professionals followed up or offered help with quitting. Greater collaboration with health professionals could result in more commercial tobacco and nicotine users becoming aware of, and receptive to, services that could increase their chances of quitting (CDC, 2015).

