Background
 The Wyoming Quit Tobacco Program (WQTP) assists enrollees in their efforts to quit using tobacco products by offering free coaching support, free nicotine replacement therapies (NRTs), and free or reduced-price prescription (Rx) medications. Under contract to the Wyoming Department of Health, Public Health Division, the Wyoming Survey & Analysis Center (WYSAC) at the University of Wyoming conducts monthly surveys of WQTP enrollees to assess quit rates and enrollee satisfaction. The survey also assesses enrollees’ use of coaching, NRTs, or prescription medications and enrollees’ opinions of different program elements. This report includes data on WQTP participants surveyed between January and June 2016, seven months after they enrolled in the WQTP. These participants enrolled in the WQTP between June and November 2015. During this period, National Jewish Health provided WQTP services in Wyoming.
The Wyoming Quit Tobacco Program (WQTP) assists enrollees in their efforts to quit using tobacco products by offering free coaching support, free nicotine replacement therapies (NRTs), and free or reduced-price prescription (Rx) medications. Under contract to the Wyoming Department of Health, Public Health Division, the Wyoming Survey & Analysis Center (WYSAC) at the University of Wyoming conducts monthly surveys of WQTP enrollees to assess quit rates and enrollee satisfaction. The survey also assesses enrollees’ use of coaching, NRTs, or prescription medications and enrollees’ opinions of different program elements. This report includes data on WQTP participants surveyed between January and June 2016, seven months after they enrolled in the WQTP. These participants enrolled in the WQTP between June and November 2015. During this period, National Jewish Health provided WQTP services in Wyoming.
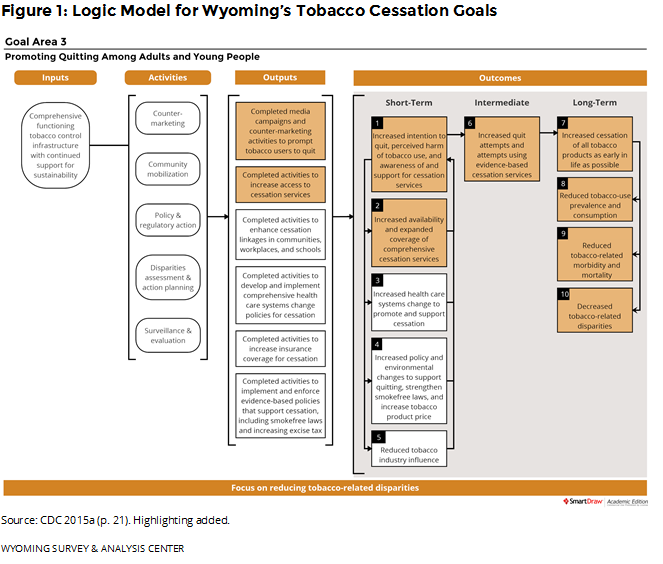
Providing cessation services to Wyoming residents is an important part of the state’s Tobacco Prevention and Control Program (TPCP). Wyoming follows the Centers for Disease Control and Prevention (CDC) guidelines for state tobacco prevention programs (CDC, 2015a). Figure 1 shows how the WQTP and the data presented in this report fit into the goals of Wyoming’s TPCP.
 Enrollee Information
Enrollee Information
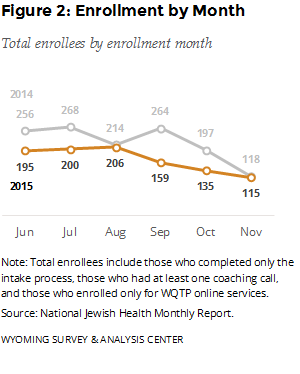
This report includes data on adult WQTP participants surveyed between January and June 2015, seven months after they enrolled in the WQTP. The follow-up participants enrolled in the WQTP between June and November 2015. How many people did WQTP serve during this time? Figure 2 provides the monthly enrollment for June – November 2015. For comparison, this figure also shows the same months from the previous year. Enrollees may sign up by completing an intake survey online or by phone. The number of enrollments between June and November was lower in 2015 than in 2014.
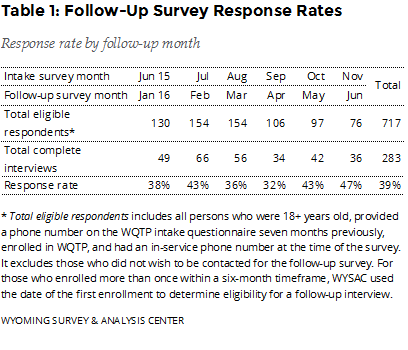
How many enrollees completed the follow-up survey? The January – June 2016 follow-up survey data include responses from 283 completed follow-up interviews (Table 1), a 39% response rate.
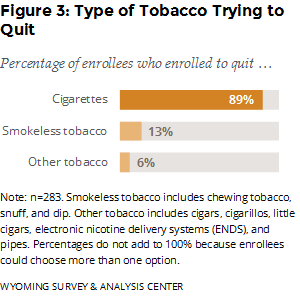
 Which type of tobacco products did enrollees get help with quitting? Enrollees could choose more than one option, but most enrolled in the WQTP to get help with quitting cigarettes (Figure 3).
Which type of tobacco products did enrollees get help with quitting? Enrollees could choose more than one option, but most enrolled in the WQTP to get help with quitting cigarettes (Figure 3).
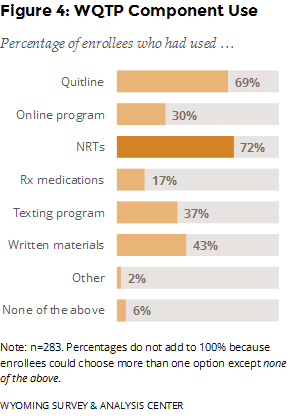
Which program components were enrollees most likely to use? NRTs, which are mailed to enrollees’ homes for free, were the most popular program component (Figure 4). Prescription medications, which require a visit to a physician, were the least popular. Most enrollees used the quitline, and almost one third used the online program. Relatively few enrollees, 16, reported not using any program component (i.e., none of the above). These enrollees may have completed the intake questionnaire without participating in any other program component. Because these responses are self-reported, respondents’ perspectives or memories about using the program may differ from National Jewish Health’s administrative records. Still, these enrollees form a useful comparison group for gauging the effectiveness of different program components.
 WQTP Outcomes
WQTP Outcomes
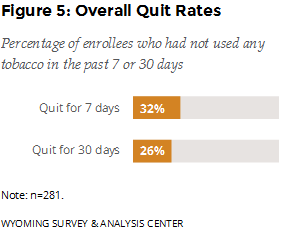
Were enrollees successful in their cessation effort? The follow-up survey asked enrollees if they had used any tobacco products in the previous seven days. If they had not, the survey asked if they had used any tobacco products in the previous 30 days. The data show that 32% of enrollees were quit for seven days; 26% were quit for 30 days (Figure 5).
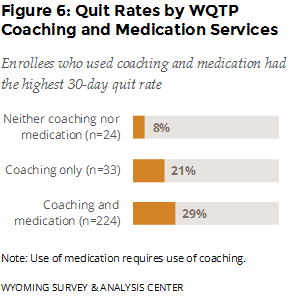 Which program component was most effective? The best outcome was associated with those who used both coaching and medication. Enrollees who used both coaching (quitline, online program, or both) and medication (NRTs, prescription, or both) had the highest 30-day quit rate (29%), seven months after enrollment (Figure 6).
Which program component was most effective? The best outcome was associated with those who used both coaching and medication. Enrollees who used both coaching (quitline, online program, or both) and medication (NRTs, prescription, or both) had the highest 30-day quit rate (29%), seven months after enrollment (Figure 6).
What is the quit rate for Chantix users? In February 2016, the WQTP began offering free Chantix to enrollees. This report does not include data on enrollees from February 2016 (or beyond), but as a baseline, 36% of enrollees (n = 22) who used Chantix (with no other NRTs or Rx medications) had been quit for 30 days. This is higher than those who used coaching only (21%) and those who used NRTs and coaching (30%).
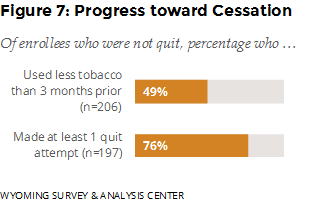
Did those who had not quit make progress toward cessation? WYSAC asked those who had not quit about changes in tobacco consumption and quit attempts (stopping the use of tobacco for 24 hours or longer since enrolling in the WQTP). Nearly half reported using less tobacco compared to three months prior to the survey, and 76% reported making at least one quit attempt since enrolling (Figure 7).
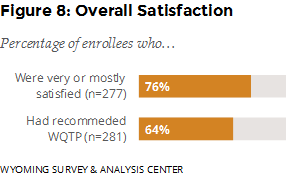
How satisfied were enrollees with the service they received from the WQTP? About one fourth (24%) were mostly satisfied and 52% were very satisfied with the WQTP. Almost two thirds (64%) reported that they had recommended the program to someone else (Figure 8).
Priority Populations
In addition to overall outcomes, this report provides follow-up data on four priority populations: those who used electronic nicotine delivery systems (ENDS), those who reported mental health conditions, those who participated in the pregnancy program, and those who participated in the American Indian Commercial Tobacco Program (AICTP).
 Alternative Nicotine Products
Alternative Nicotine Products
Electronic nicotine delivery systems (ENDS) such as e-cigarettes, e-hookahs, or vape pens are battery-operated devices that simulate smoking but do not involve the burning of tobacco. The heated vapor produced by ENDS often contains nicotine and comes in different flavors.
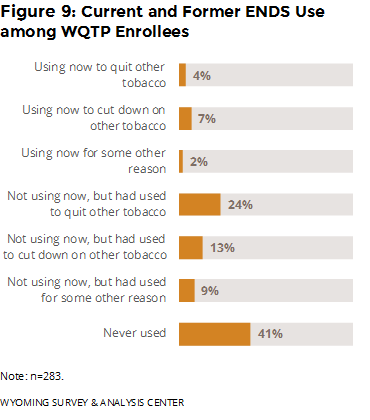
Have enrollees ever used ENDS or other similar nicotine products? If so, why did they use them? Over half of enrollees had used ENDS in their lifetime (Figure 9). Moreover, 81% of enrollees who had used ENDS used them to quit or cut-down on other tobacco, although they are not approved as cessation aids by the U.S. Food and Drug Administration (FDA, 2016).
Only 1% of enrollees had used another smoke-free form of nicotine (such as Nicogel, Camel strips, and orbs) that is not approved as a smoking cessation product.
Mental Health
Studies (e.g., CDC, 2013; Talati, Keyes, & Hasin, 2016) have demonstrated an association between cigarette smoking and mental health conditions. People with mental health conditions are more likely to smoke and to smoke more cigarettes than people without mental health conditions (CDC, 2013). Based on combined data from the 2009-2011 National Survey on Drug Use and Health (NSDUH), 36.7% of Wyoming adults who had a mental health condition had smoked part or all of a cigarette within the 30 days prior to being surveyed, compared to 22.8% of Wyoming adults without a mental health condition (CDC, 2013).
 Enrollees who completed the intake survey over the phone answered questions about their mental health. The WQTP online intake form has included these questions since August 28, 2015. For this reason, the results below do not apply to enrollees who used the online program only before August 28, 2015.
Enrollees who completed the intake survey over the phone answered questions about their mental health. The WQTP online intake form has included these questions since August 28, 2015. For this reason, the results below do not apply to enrollees who used the online program only before August 28, 2015.
The intake questionnaire asks, “Do you have any mental health conditions, such as anxiety disorder, depression disorder, bipolar disorder, alcohol/drug abuse,2 or schizophrenia?” WYSAC merged responses to this mental health question at intake with the follow-up survey data, which resulted in 234 follow-up survey respondents who had answered the question. Of these respondents, 46% said they had a mental health condition at the time of the intake survey.
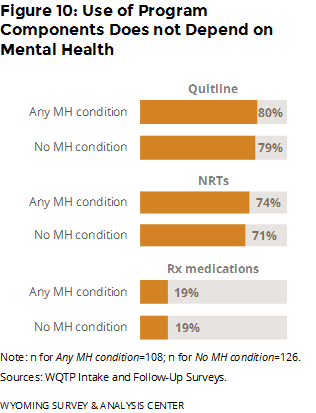
How did program usage rates differ for enrollees who reported mental health conditions? Enrollees who reported mental health conditions used program components at about the same rates as those who did not report mental health conditions (Figure 10).
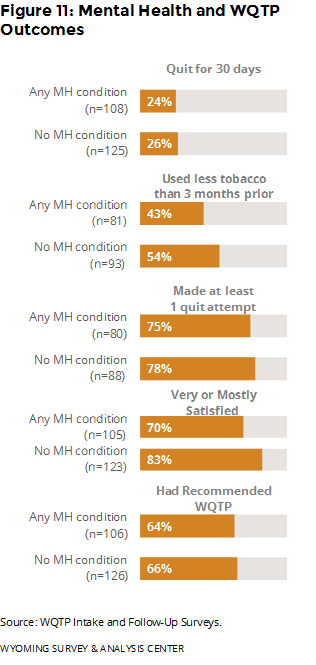 Did outcomes differ for people with mental health conditions? Those without mental health conditions were more likely to have used less tobacco and to have been satisfied with the WQTP. However, those with and without mental health conditions were about equally likely to have been quit for 30 days, to have made at least one quit attempt, and to have recommended the WQTP (Figure 11).
Did outcomes differ for people with mental health conditions? Those without mental health conditions were more likely to have used less tobacco and to have been satisfied with the WQTP. However, those with and without mental health conditions were about equally likely to have been quit for 30 days, to have made at least one quit attempt, and to have recommended the WQTP (Figure 11).
Pregnant Women
Smoking is linked to complications during pregnancy, including miscarriage and birth defects (CDC, 2015b). These excess risks make pregnant women a priority population for the Wyoming TPCP. How did pregnant women perform in their cessation efforts?
Five of the 20 enrollees who said they were pregnant at the time of enrollment responded to the follow-up survey. All five had enrolled in the specialty program for pregnant women. One pregnant woman had been quit for at least 30 days prior to being surveyed. The other four were using tobacco at the time they were surveyed. Three of these four reported using less tobacco than three months prior and making at least one quit attempt since enrolling. The small sample size means that it is not possible to generalize the results to all pregnant WQTP enrollees.
American Indians
On August 1, 2015, National Jewish Health began offering the American Indian Commercial Tobacco Program (AICTP) to provide a culturally-sensitive approach to help American Indians quit commercial tobacco use (National Jewish Health, 2015).
Two of eight American Indians in Wyoming who enrolled in the AICTP completed the follow-up survey. One of them had been quit for at least 30 days prior to being surveyed. The other respondent was using tobacco products at the time of follow-up, but reported using less tobacco than three months prior and had made at least one quit attempt since enrolling. The small sample size means that it is not possible to generalize the results to all American Indian enrollees.
 Enrollee Reports on Strengths and Weaknesses of the WQTP
Enrollee Reports on Strengths and Weaknesses of the WQTP
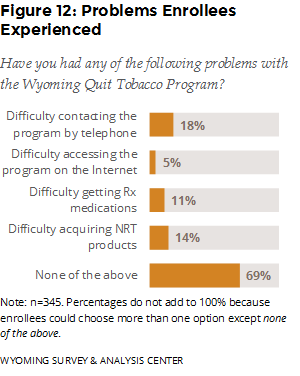
What did enrollees report about the strengths and weaknesses of the WQTP? Most enrollees (69%) reported no problems with the core program components (Figure 12). Among those who reported difficulty, contacting the program by telephone was the most problematic, followed by acquiring NRT products.